Patient Health Questionnaire 9 (PHQ-9)
Recommended frequency: Every 2 weeks
Summary
The Patient Health Questionnaire 9 (“PHQ-9”) is a multi-purpose measure used to identify and monitor depression severity. It is a brief, 9-item version of the original PHQ assessment, which measures a variety of mental health challenges in addition to depression, such as anxiety, panic disorder, sleep disorders, and more. The PHQ-9 was co-created by Drs. Robert L. Spitzer, Janet W.B. Williams and Kurt Kroenke in 1999.
About the PHQ-9
The PHQ-9 combines depression diagnostic criteria from the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) with other leading major depressive symptoms. The key diagnostic symptom criteria adapted from the DSM-IV includes:
- Two typical signs of depression: anhedonia (referring to the inability or reduced ability to experience pleasure) and depressed mood;
- Cognitions (e.g. guilt/worthlessness and suicidality/thoughts of death); and
- Physical symptoms (e.g. change in appetite, difficulty sleeping and concentrating, feeling tired/slowed down or restless).
Each of the 9 questions rate the frequency of the symptoms, which factors into the severity index.
Clinicians and clinical leaders will often ask about the differences between the PHQ-9 and other depression scales. In comparison to the other commonly used depression scales (BDI, HAD-D, QIDS), the confidence intervals are quite similar, meaning they have all demonstrated reliability, validity, and are responsive to change. The PHQ-9 has a particularly high validity score, such that when PHQ-9 scores were above 10, the measure was shown to have a sensitivity of 88% and a specificity of 88% for Major Depressive Disorder—meaning that a score above 10 was a good indication that a diagnosis of depression would occur. Each of the major depression scales have their differences, although the PHQ-9 and BDI-II in particular tend to measure relatively equal levels of severity and track symptom change in a similar manner. The PHQ-9 is often preferred to other comparable assessments due to its brevity, which makes it easy to integrate into research or practice, and helps promote high completion rates.
Who is the PHQ-9 Assessment for?
Review the list below to determine if this assessment should be used with your client. If you answer NO to all four questions, the PHQ-9 is a good fit to use with your client.
- Is your client experiencing normal bereavement?
- Does your client have a history of Manic Episodes (Bipolar Disorder)?
- Does your client have a physical disorder or are they taking medication, or other drugs that may be the biological cause of the depressive symptoms?
- Is your client under 18? If they are, please refer to the Child Depression & Anxiety (RCADS 25) measure or the Child Depression (CES-DC) measure.
Note: The PHQ-9 can also be used for patients with stroke, and is suitable for geriatric patients, patients with traumatic brain injury, in primary care and obstetrics-gynaecology settings, and with members of the general population.
The Scale
The scale is made up of 9 items that target symptoms of major depressive disorder. Since this assessment relies on clients to self-report, it’s important that you verify the answers with them in session to ensure they understood each question, and to gather any other relevant information and context they provide about their symptoms and experience.
The PHQ-9 requires the client to provide answers based on how often they experienced the below challenges, over the course of the last 2 weeks.
Scoring the PHQ-9
A diagnosis of Major Depressive Disorder should be considered if there are 5 or more items that score in the shaded section, with one of these items being #1 or #2.
Other depressive disorders should be considered if the client presents 2-4 items in the shaded section, with one corresponding to #1 or #2.
You can then determine the severity by adding up the overall score:
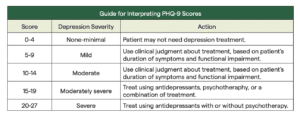
Depression severity is calculated by assigning scores of 0, 1, 2, and 3, to the response categories of “not at all”, “several days”, “more than half the days”, and “nearly every day”, respectively. The PHQ-9 total score for the nine items ranges from 0 to 27. The table below outlines the score groupings and proposed treatment actions. Scores of 5, 10, 15, and 20 represent respective cutpoints for mild, moderate, moderately severe and severe depression. The PHQ-9 is also sensitive to change, meaning depression severity and symptom frequency that increases or decreases during treatment can be recorded through regular, repeat assessments.
Ultimately, the higher a client scores, the more severe their depression is.
Note: Question 9 is a single screening question to identify suicide risk. Any client who answers ‘yes’ to question 9 needs further assessment to determine their risk level and inform the appropriate next steps. When this assessment is completed on the Greenspace platorm, a [insert flag from GS system] and date of response are placed the client profile to highlight suicidality, which indicates that the client has scored 1 or above on this PHQ-9 item or another measure that monitors for this risk.
TIP: When discussing scores with clients, it’s important to remind them that even if they do not meet severe criteria, it does not mean their symptoms are any less valid. This is a good opportunity to dig in to each symptom they report, in order to identify other potential root causes, work on coping mechanisms, and to inform treatment goals and approach moving forward.
Practice: PHQ-9 Three Ways
The ‘PHQ-9 Three-Ways’ exercise is used by our partners at the Yale Measurement-Based Care Collaborative to help clinicians feel comfortable exploring assessment results with clients and getting curious about what the scores mean. This process is key to driving collaborative discussions with clients and helping to inform treatment decisions.
During our second panel with the Yale MBCC attendees participated in this practice exercise. The Yale MBCC team shared example PHQ-9 scores from three different clients, each with slightly different responses. Attendees then reviewed the responses and shared what they noticed, what hypotheses they were forming, and what they might ask the client in session to dig deeper into their experience.
Watch this clip for guidance on how to practice interpreting PHQ-9 results for yourself or your clinical team:
Learn more about this exercise and some of the key takeaways from the session here.
Copyright Information
Developed by Drs. Robert L. Spitzer, Janet B. W. Williams, Kurt Kroenke and colleagues. No permission required to reproduce, translate, display or distribute.
References
American Psychological Association. (2020, June). Patient Health Questionnaire (PHQ-9 & PHQ-2). https://www.apa.org/pi/about/publications/caregivers/practice-settings/assessment/tools/patient-health
Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine, 16(9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Disclaimer
The information provided above was derived from materials and research developed by the creators and/or licensors of the BR-WAI. The information may not be exhaustive and is not a treatment recommendation by Greenspace.
Assessment Insights
Check out more than 40 Assessment Guides with information and insights on the most popular assessments used on the Greenspace MBC Platform. Explore the categories below to find assessments you may be interested in learning more about.
Back to the hub